Nourishment without disruption: tips for maintaining continuity of care
Parenteral nutrition (PN) is a complex therapy that may be administered to patients at any age in a variety of clinical settings, including hospitals, long-term care (LTC) facilities, and at home.1 Because it is classified as a high-alert medication by the Institute for Safe Medication Practices,2,3 PN requires an interdisciplinary approach to help mitigate potential risks and complications associated with its use.1 This is especially important when patients who are receiving PN are transferred from one clinical setting to another.
Established coordination and clear communication are key to facilitating successful transitions from4:
- One medical unit to another within a hospital
- A hospital to a skilled nursing facility, LTC facility, or home
- A skilled nursing facility, LTC facility, or home to a hospital
Care transitions come with challenges
Transitions of care pose several challenges not only for healthcare providers and organizations but for patients and caregivers.4 It’s been shown that hospital discharge is associated with risks that cause medical errors and adverse events that can lead to readmission and/or complications.4,5 These include failure of communication, insufficient patient education, lack of timely follow-up, and inadequate home services.5 While these things can negatively impact a patient’s journey on PN, there are steps that can be taken to achieve a transition of care that is safe and successful.
“When a high-alert medication such as PN is involved, risk-avoidance strategies require standardized processes with excellent communication between all members of the team, including healthcare providers from the sending and receiving organization/setting who have a high degree of competence in their respective roles as well as the patient/caregiver.”4
From: Adams SC, et al. Nutr Clin Pract. 2022;37(3):493-508.
Considerations for navigating transitions of care for PN patients
When it comes to transferring patients, safety is the top priority. Unfortunately, medication errors affect almost every patient whose care is transitioned to another clinical setting.6 To reduce the risk of these errors, a standardized process should be considered to ensure all aspects of the transition are addressed.4
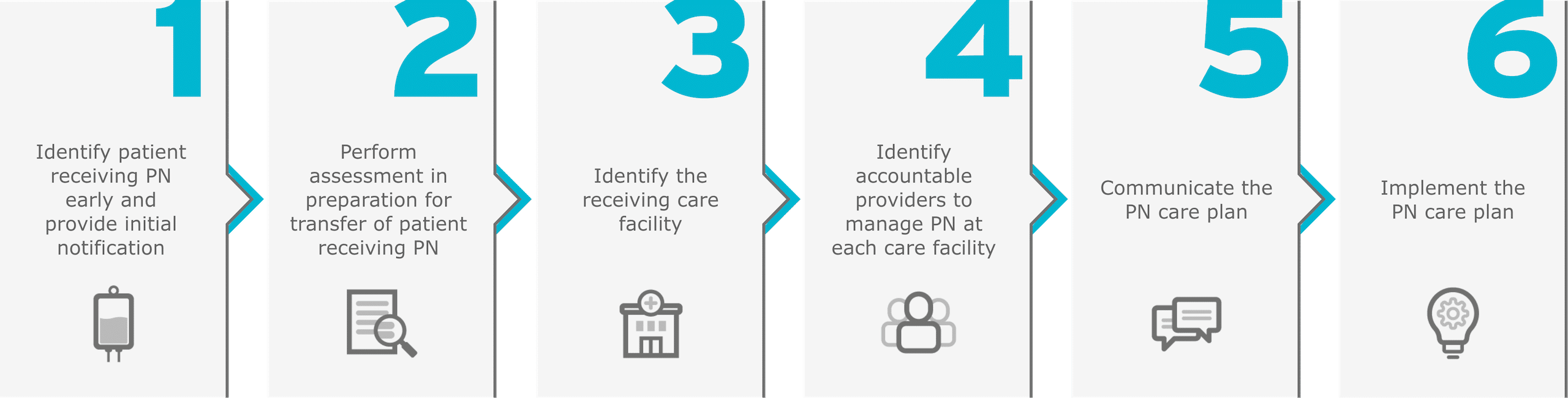
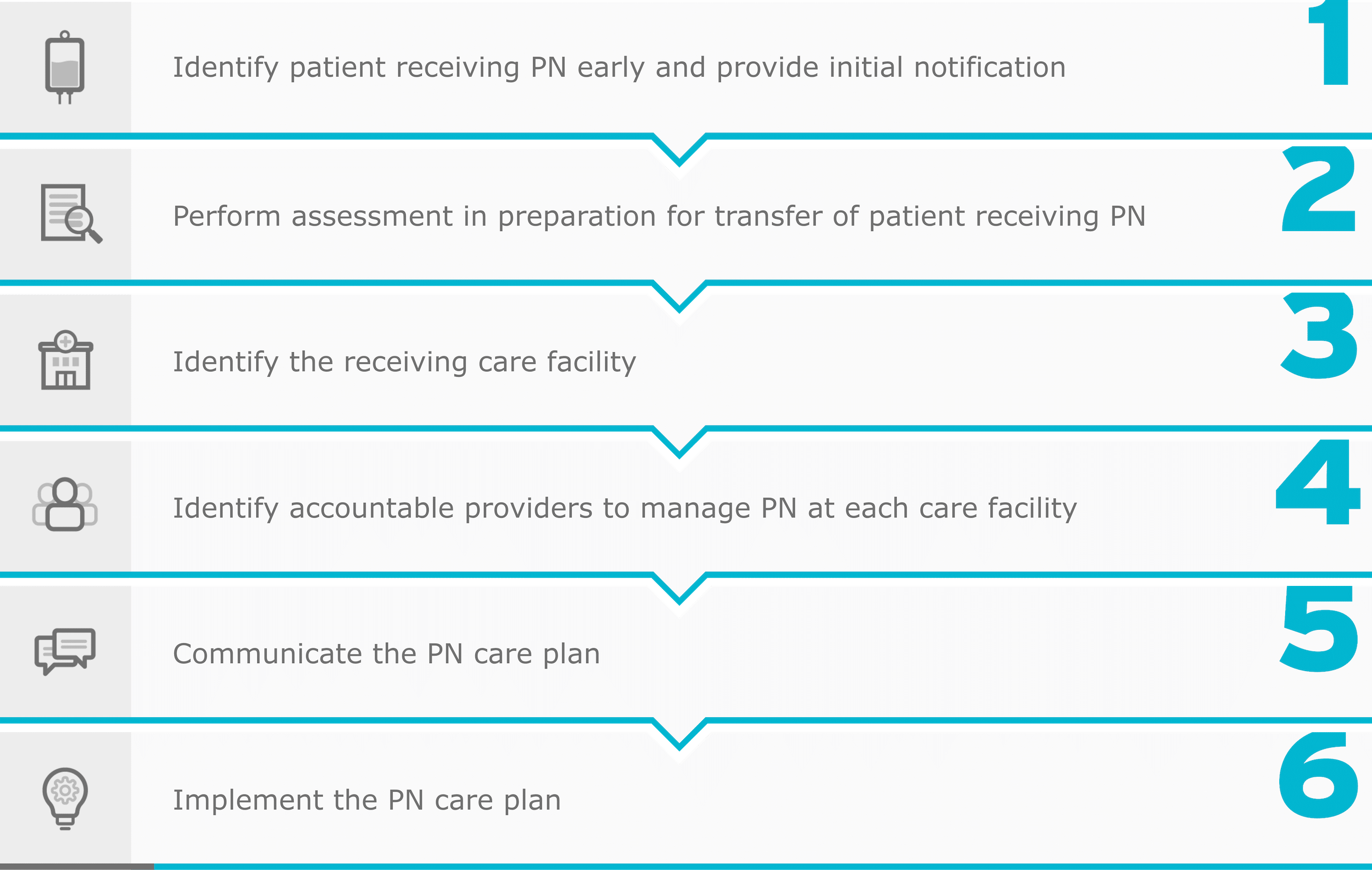
Phases in the transition process4
Adapted from: Adams SC, et al. Nutr Clin Pract. 2022;37(3):493-508.
This sample checklist is just one step toward creating a systematic approach to transitioning PN patients from one clinical setting to another4:
-
- Evaluate the necessity of PN based on medical condition, nutritional requirements, and anticipated duration
-
- Assign responsibilities to team members involved in the transition process, including physicians, nurses, pharmacists, dietitians, and home healthcare providers
-
- Conduct a thorough review of the patient’s current medications and allergies, ensuring compatibility and safety of PN
-
- Schedule follow-up appointments with healthcare providers, including physicians, dietitians, and pharmacists, to monitor the patient’s progress and adjust PN therapy as needed
-
- Provide comprehensive education to the patient and caregivers regarding PN administration, equipment uses, and signs of complications
- Address nutritional needs, dietary restrictions, and lifestyle modifications
-
- Verify the availability of PN products and supplies needed for home administration
- Make adjustments to the PN order as necessary, considering formulary differences and addressing any product shortages
- Communicate changes with the care team and ensure proper documentation
-
- Verify and review the PN order to ensure it is appropriate, accurate, complete, stable, and compatible
- Ensure adherence to aseptic techniques and proper handling of PN components
-
- Develop protocols for preventing central line-associated bloodstream infections (CLABSIs), including catheter care, dressing changes, and sterile techniques
- Educate caregivers on infection prevention measures and early signs of infection
-
- Develop contingency plans for potential complications or readmissions related to PN therapy
- Communicate these plans to the patient, caregivers, and healthcare providers involved in the transition process
-
- Monitor the clinical outcomes and financial implications of the transition process
- Identify and address any challenges or barriers to successful transition, considering both clinical and financial factors
Careful coordination, recognizing challenges that may present during transitions of care, and following the necessary policies and procedures can all help reduce the risk of errors that may lead to patient harm.4 Every team member and every stage of the process is critical to ensuring a smooth and successful care transition for healthcare providers, their patients receiving PN, and caregivers.4