We develop innovations that nourish patients who need PN

See how Fresenius Kabi Nutrition may help your critically and chronically ill patients with its portfolio of clinical nutrition products.

We’re proud to support marine conservation by ensuring that the fish oil in our products is sustainably sourced.
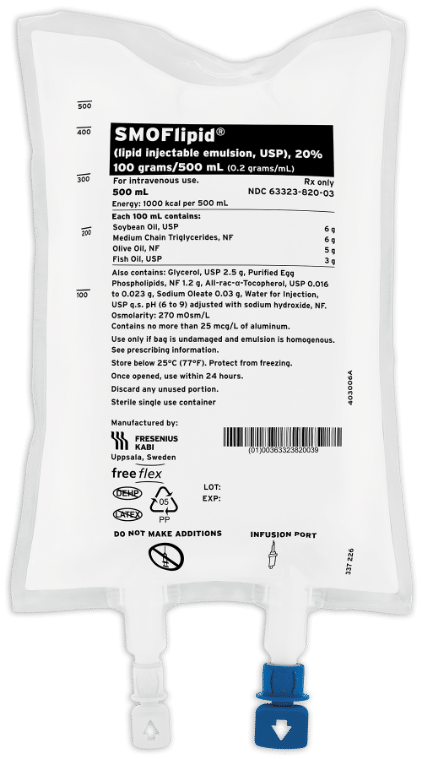
The first 4-oil lipid emulsion for adult and pediatric patients, including term and preterm neonates, in the US1
With SMOFlipid, Fresenius Kabi supported PN and critical care medical societies’ need for an alternative to soy-based lipid injectable emulsions. This blend of soybean oil, medium-chain triglycerides (MCT), olive oil, and fish oil is the FIRST and ONLY advancement in US lipid emulsions for adults in more than 40 years.
- Administered to more than 7 million patients worldwide* for over 15+ years
- Well-established safety and tolerability profile1
- The fatty acid ratio in SMOFlipid is in line with expert recommendations for adults2-5
The first and only fish oil lipid emulsion for pediatric patients with parenteral nutrition-associated cholestasis (PNAC) in the US1
Omegaven is a PN product rich in omega-3s that became commercially available for pediatric patients in November of 2018; Omegaven was previously available only for compassionate care. Fresenius Kabi was aware of the need for this product to be more broadly available to pediatric patients and worked hard to secure the necessary clinical evidence to support FDA approval.
- Omegaven is a source of calories and fatty acids in pediatric patients with PNAC1
- Fish oil is the newest type of lipid to be introduced into PN products
- Fish oil is rich in omega-3s
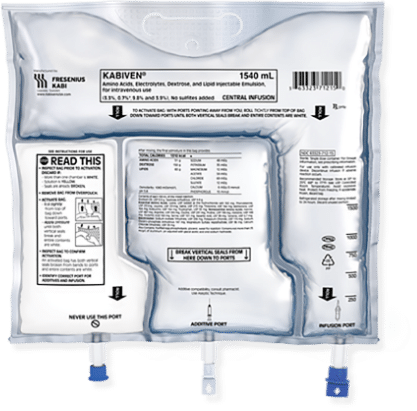
The first 3-chamber bag for PN for adults
Kabiven/Perikabiven’s unique design streamlines the delivery of nutrition therapy to patients by simplifying calculations, prescription writing, compounding, and administration, all while supporting PN safety by minimizing the risk of contamination.1 The Kabiven and Perikabiven 3-chamber PN bags help clinicians efficiently deliver 3 macronutrients (dextrose, protein, and lipids) plus electrolytes in volumes and concentrations that meet the needs of most PN patients.2,3
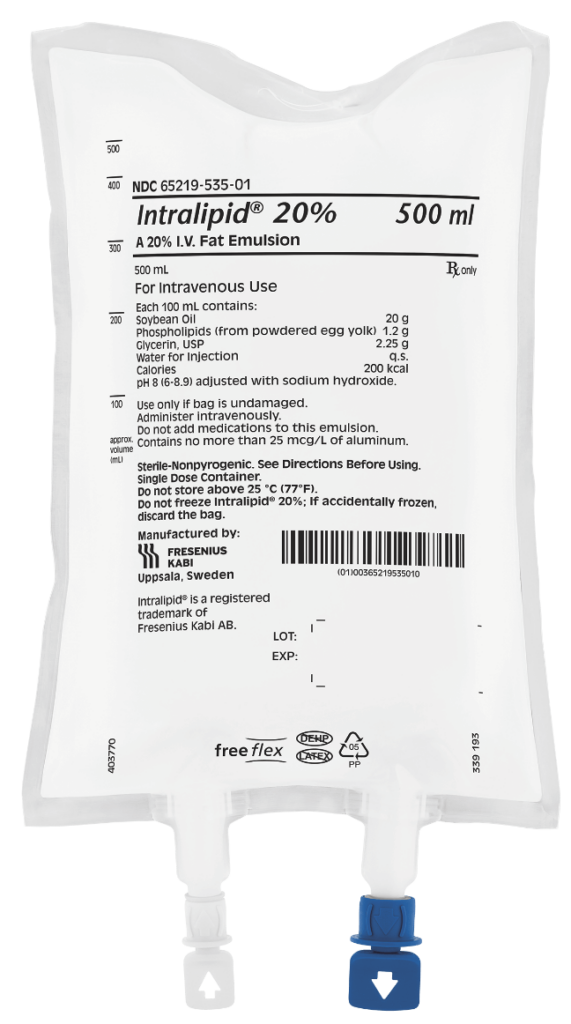
A long-standing and chosen lipid worldwide
Intralipid is a 100% soybean oil-based ILE, which has been administered in more than 200 million infusions since its European approval in 1962.*
Intralipid may be considered for patients requiring PN1:
- As a source of essential fatty acids for prevention of essential fatty acid deficiency
- When other lipid sources are not an option
- For inpatient use in both adults and children
KabiCare Patient Support Program for Parenteral Nutrition
Fresenius Kabi’s patient support program, KabiCare, offers online resources for claims appeals and billing as well as coding guides for parenteral nutrition.
The omega-3 difference
Angling for more information about fish oil and omega-3s in PN?
For Consumers
SMOFLIPID® (lipid injectable emulsion USP), for intravenous use
IMPORTANT SAFETY INFORMATION
What is SMOFlipid?
- Indicated in adult and pediatric patients as a source of calories and essential fatty acids for parenteral nutrition (PN) when oral or enteral nutrition is not possible, insufficient, or contraindicated.
- The hourly infusion rate in pediatrics should not exceed 0.75 mL/kg/hour and 0.5 mL/kg/hour in adults.
SMOFlipid should not be received by patients who have:
- A known allergy to fish, egg, soybean, or peanut, or to any of the active or inactive ingredients in SMOFlipid.
- Abnormally high levels of lipid (triglycerides) in the blood.
SMOFlipid may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Parenteral nutrition-associated liver disease (PNALD) may progress to liver inflammation and damage caused by a buildup of fat in the liver with scarring and cirrhosis.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides (Hypertriglyceridemia): Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels.
Monitoring/Laboratory Tests: The content of vitamin K may interfere with blood clotting activity of medications.
The most common side effects (>1%) in adult patients include nausea, vomiting, and high levels of glucose in the blood and in pediatric patients include low levels of red blood cells, vomiting, increased levels of liver enzymes (i.e., gamma-glutamyltransferase) and hospital-acquired infections.
These are not all the possible side effects associated with SMOFlipid. Call your healthcare provider for medical advice regarding SMOFlipid side effects. You are encouraged to report negative side effects of SMOFlipid. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling can be found at https://www.FreseniusKabiNutrition/SMOFlipidPI.
For Healthcare Professionals
SMOFLIPID (lipid injectable emulsion, USP), for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
SMOFlipid is indicated in adult and pediatric patients, including term and preterm neonates, as a source of calories and essential fatty acids for parenteral nutrition (PN) when oral or enteral nutrition is not possible, insufficient, or contraindicated.
IMPORTANT SAFETY INFORMATION
For intravenous infusion only into a central or peripheral vein. Use a non-vented non-DEHP 1.2 micron in-line filter set during administration. Recommended dosage depends on age, energy expenditure, clinical status, body weight, tolerance, ability to metabolize and eliminate lipids, and consideration of additional energy given to the patient. The recommended dose for adults and pediatrics is shown in Table 1. For information on age-appropriate infusion rate, see the full prescribing information. SMOFlipid Pharmacy Bulk Package is only indicated for use in pharmacy admixture programs for the preparation of three-in-one or total nutrition admixtures. Protect the admixed PN solution from light.
Table 1: Recommended Adult and Pediatric Dosage
| Age | Nutritional Requirements | |
|---|---|---|
| Initial Recommended Dosage | Maximum Dosage | |
| Birth to 2 years of age (including preterm and term neonates) |
0.5 to 1 g/kg/day | 3 g/kg/day |
| Pediatric patients 2 to <12 years of age | 1 to 2 g/kg/day | 3 g/kg/day |
| Pediatric patients 12 to 17 years of age | 1 g/kg/day | 2.5 g/kg/day |
| Adults | 1 to 2 g/kg/day | 2.5 g/kg/day |
SMOFlipid is contraindicated in patients with known hypersensitivity to fish, egg, soybean, peanut, or any of the active or inactive ingredients, and severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglycerides >1,000 mg/dL).
Clinical Decompensation with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who received parenteral nutrition for greater than 2 weeks, especially preterm neonates. Monitor liver tests; if abnormalities occur consider discontinuation or dosage reduction.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reactions occur.
Risk of Infections, Fat Overload Syndrome, Refeeding Syndrome, Hypertriglyceridemia, and Essential Fatty Acid Deficiency: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm neonates.
Most common adverse drug reactions (≥5%) from clinical trials in adults were nausea, vomiting, and hyperglycemia. Most common adverse drug reactions (≥5%) from clinical trials in pediatric patients were anemia, vomiting, increased gamma-glutamyltransferase, and nosocomial infection.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use SMOFlipid safely and effectively. Please see full prescribing information for SMOFlipid (lipid injectable emulsion, USP), for intravenous use at www.FreseniusKabiNutrition.com/SMOFlipidPI.
For Consumers
OMEGAVEN (fish oil triglycerides) injectable emulsion, for intravenous use
IMPORTANT SAFETY INFORMATION
These highlights do not include all the information needed to use OMEGAVEN safely and effectively. To learn more about OMEGAVEN for your child, talk to your child’s healthcare provider. OMEGAVEN is available by prescription only. The FDA-approved product labeling can be found at www.freseniuskabinutrition.com/OmegavenPI.
What is OMEGAVEN?
- A fish oil-based intravenous lipid emulsion that is a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis (PNAC).
- Does not prevent PNAC.
- It has not been demonstrated that the clinical outcomes seen in pediatric patients are a result of the omega-6:omega-3 fatty acid ratio of the product.
- The hourly infusion rate should not exceed 1.5 mL/kg/hour
OMEGAVEN should not be received by patients who have:
- a known allergy to fish or egg protein or to any of the ingredients in OMEGAVEN.
- a severe bleeding disorder.
- abnormally high levels of lipid (triglycerides) in the blood.
What important safety information should I know about OMEGAVEN?
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides (Hypertriglyceridemia): Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels.
The most common side effects, (>15%) include: vomiting, agitation, slower than normal heartbeat, interruption of breathing, and viral infection.
These are not all the possible side effects associated with OMEGAVEN. Call your healthcare provider for medical advice regarding OMEGAVEN side effects. You are encouraged to report negative side effects of OMEGAVEN. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling can be found at www.FreseniusKabiNutrition.com/OmegavenPI.
For Healthcare Professionals
OMEGAVEN (fish oil triglycerides) injectable emulsion, for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
Omegaven is indicated as a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis (PNAC).
Limitations of Use
Omegaven is not indicated for the prevention of PNAC. It has not been demonstrated that Omegaven prevents PNAC in parenteral nutrition (PN)-dependent patients.
It has not been demonstrated that the clinical outcomes observed in patients treated with Omegaven are a result of the omega-6: omega-3 fatty acid ratio of the product.
IMPORTANT SAFETY INFORMATION
Protect the admixed PN solution from light. Prior to administration, correct severe fluid and electrolyte disorders and measure serum triglycerides to establish a baseline level. Initiate dosing in PN-dependent pediatric patients as soon as direct or conjugated bilirubin levels are 2 mg/dL or greater. The recommended nutritional requirements of fat and recommended dosages of Omegaven to meet those requirements for pediatric patients are provided in Table 1, along with recommendations for the initial and maximum infusion rates. Administer Omegaven until direct or conjugated bilirubin levels are less than 2 mg/dL or until the patient no longer requires PN.
Table 1: Recommended Pediatric Dosage and Infusion Rate
| Nutritional Requirements | Direct Infusion Rate | |
|---|---|---|
| Initial | Maximum | |
| 1 g/kg/day; this is also the maximum daily dose | 0.2 mL/kg/hour for the first 15 to 30 minutes; gradually increase to the required rate after 30 minutes |
1.5 mL/kg/hour |
Omegaven is contraindicated in patients with known hypersensitivity to fish or egg protein or to any of the active ingredients or excipients, severe hemorrhagic disorders due to a potential effect on platelet aggregation, severe hyperlipidemia or severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglyceride concentrations greater than 1,000 mg/dL).
Clinical Decompensation with Rapid Infusion of Lipid Injectable Emulsions in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported. Hypertriglyceridemia was commonly reported. Strictly adhere to the recommended total daily dosage; the hourly infusion rate should not exceed 1.5 mL/kg/hour. Carefully monitor the infant’s ability to eliminate the infused lipids from the circulation (e.g., measure serum triglycerides and/or plasma free fatty acid levels). If signs of poor clearance of lipids from the circulation occur, stop the infusion and initiate a medical evaluation.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reaction occurs.
Infections, Fat Overload Syndrome, Refeeding Syndrome, and Hypertriglyceridemia: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm infants.
Monitoring and Laboratory Tests: Routine laboratory monitoring is recommended, including monitoring for essential fatty acid deficiency.
The most common adverse drug reactions (>15%) are: vomiting, agitation, bradycardia, apnea and viral infection.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use Omegaven safely and effectively. Please see full prescribing information for Omegaven (fish oil triglycerides) injectable emulsion for intravenous use at www.freseniuskabinutrition.com/OmegavenPI.
For Consumers
KABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
PERIKABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
IMPORTANT SAFETY INFORMATION
What is Kabiven and Perikabiven?
- Indicated in adult patients as a source of calories, protein, electrolytes and essential fatty acids for parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. Kabiven and Perikabiven may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adults.
- Do not exceed the recommended maximum infusion rate of 2.6 mL/kg/hour for Kabiven and 3.7 mL/kg/hour for Perikabiven.
Limitations of Use
Neither Kabiven nor Perikabiven is recommended in pediatric patients less than 2 years old because the fixed amount of the formulations do not meet nutritional needs in this age group.
Do not use Kabiven or Perikabiven in patients who have:
- Simultaneous treatment with ceftriaxone in neonates (28 days of age or younger)
- Known allergy to egg, soybean, peanut or any of the active or inactive ingredients
- Abnormally high levels of lipid (triglycerides) in the blood (with serum triglyceride concentration >1,000 g/dL)
- Inborn errors of amino acid metabolism (a genetic defect in protein metabolism)
- Cardiopulmonary instability (inability for the heart and lungs to function right)
- Hemophagocytic syndrome (a disorder of the immune system)
Kabiven and Perikabiven may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who receive parenteral nutrition for greater than 2 weeks. Your healthcare provider will monitor liver tests.
- Pulmonary Embolism (a blockage in a blood vessel in the lung) and Respiratory Distress (increased breathing rate, bluish skin color changes, wheezing) due to Pulmonary Vascular Precipitates (solid substance in the blood vessel of the lungs): If signs of lung issues occur, stop the infusion and start a medical evaluation.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction
- Precipitation (solid substance in the blood vessel) with Ceftriaxone: Do not administer ceftriaxone simultaneously with Kabiven or Perikabiven via a Y-site.
- Infection, fat overload, hyperglycemia (high blood sugar) and refeeding syndrome: Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels
The most common adverse reactions for Kabiven (≥3%) are nausea, fever, high blood pressure, vomiting, decreased blood hemoglobin, decreased blood total protein, low blood potassium, and increased gamma glutamyltransferase (a liver enzyme). The most common adverse reactions for Perikabiven (≥3%) are high blood sugar, low blood potassium, fever and increased blood lipids.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Tell your doctor if you are taking coumarin and coumarin derivatives, including warfarin: the drug activity may be lessened and your healthcare provider will monitor your blood.
These are not all the possible side effects associated with Kabiven and Perikabiven. Call your healthcare provider for medical advice regarding Kabiven and Perikabiven side effects. You are encouraged to report negative side effects of Kabiven and Perikabiven. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling for KABIVEN® (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use and PERIKABIVEN® (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use can be found at www.FreseniusKabiNutrition.com/KabivenPI and www.FreseniusKabiNutrition.com/PerikabivenPI.
For Healthcare Professionals
KABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
PERIKABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
KABIVEN and PERIKABIVEN are each indicated as a source of calories, protein, electrolytes and essential fatty acids for adult patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. KABIVEN and PERIKABIVEN may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adult patients.
Limitations of Use
Neither KABIVEN nor PERIKABIVEN is recommended for use in pediatric patients <2 years including preterm infants because the fixed content of the formulation does not meet nutritional requirements in this age group.
IMPORTANT SAFETY INFORMATION
KABIVEN is indicated for intravenous infusion into a central vein. PERIKABIVEN is indicated for intravenous infusion into a peripheral or central vein. It is recommended to mix the contents thoroughly by inverting the bags upside down to ensure a homogenous admixture. Ensure the vertical seals between chambers are broken and the contents of all three chambers for KABIVEN and PERIKABIVEN are mixed together prior to infusion. The dosage of KABIVEN and PERIKABIVEN should be individualized based on the patient’s clinical condition (ability to adequately metabolize amino acids, dextrose and lipids), body weight and nutritional/fluid requirements, as well as additional energy given orally/enterally to the patient. Prior to administration of KABIVEN and PERIKABIVEN, correct severe fluid, electrolyte and acid-base disorders. Before starting the infusion, obtain serum triglyceride levels to establish the baseline value. Do not exceed the recommended maximum infusion rate of 2.6 mL/kg/hour for KABIVEN and 3.7 mL/kg/hour for PERIKABIVEN.
KABIVEN and PERIKABIVEN are contraindicated in:
- Concomitant treatment with ceftriaxone in neonates (28 days of age or younger)
- Known hypersensitivity to egg, soybean, peanut, or any of the active or inactive ingredients.
- Severe disorders of lipid metabolism characterized by hypertriglyceridemia (with serum triglyceride concentration >1,000 g/dL).
- Inborn errors of amino acid metabolism.
- Cardiopulmonary instability
- Hemophagocytic syndrome
Clinical Decompensation with Rapid Infusion of Lipid Injectable Emulsions in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who receive parenteral nutrition for greater than 2 weeks. Monitor liver tests; if abnormalities occur, consider discontinuation or dosage reduction.
Pulmonary Embolism and Respiratory Distress due to Pulmonary Vascular Precipitates: If signs of pulmonary distress occur, stop the infusion and initiate a medical evaluation.
Hypersensitivity reactions: Monitor for signs or symptoms and discontinue infusion if reactions occur.
Precipitation with Ceftriaxone: Do not administer ceftriaxone simultaneously with KABIVEN or PERIKABIVEN via a Y-site.
Infection, fat overload, hyperglycemia and refeeding complications: Monitor for signs and symptoms; monitor laboratory parameters.
The most common adverse reactions for KABIVEN (≥3%) are nausea, pyrexia, hypertension, vomiting, decreased hemoglobin, decreased total protein, hypokalemia, decreased potassium, and increased gamma glutamyltransferase. The most common adverse reactions for PERIKABIVEN (≥3%) are hyperglycemia, hypokalemia, pyrexia, and increased blood triglycerides.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Coumarin and coumarin derivatives, including warfarin: Anticoagulant activity may be counteracted; monitor laboratory parameters
This Important Safety Information does not include all the information needed to use KABIVEN and PERIKABIVEN safely and effectively. Please see full prescribing information for KABIVEN and PERIKABIVEN (amino acids, electrolytes, dextrose and lipid injectable emulsion), for intravenous use at www.FreseniusKabiNutrition.com/KabivenPI and www.FreseniusKabiNutrition.com/PerikabivenPI.
For Consumers
Intralipid (lipid injectable emulsion) for intravenous use
IMPORTANT SAFETY INFORMATION
What is Intralipid?
- Indicated as a source of calories and essential fatty acids for adult and pediatric patients requiring parenteral nutrition (PN) and as a source of essential fatty acids for prevention of essential fatty acid deficiency (EFAD).
Intralipid should not be received by patients who have:
- A known allergy to egg, soybean, or peanut, or any of the active ingredients or excipients in Intralipid.
- Abnormally high levels of lipid (triglycerides) in the blood.
Intralipid may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly adhere to the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Parenteral nutrition-associated liver disease (PNALD) may progress to liver inflammation and damage caused by a buildup of fat in the liver with scarring and cirrhosis.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides: Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels
Monitoring/Laboratory Tests: The content of vitamin K may interfere with blood clotting activity of medications.
The most common side effects (≥5%) in adult patients include nausea, vomiting and fever and in pediatric patients include low levels of red blood cells, vomiting, increased levels of liver enzymes (i.e., gamma-glutamyltransferase), and cholestasis (i.e., reducing or blocking the flow of bile).
These are not all the possible side effects associated with Intralipid. Call your healthcare provider for medical advice regarding Intralipid side effects. You are encouraged to report negative side effects of Intralipid. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling for Intralipid® 20% (lipid injectable emulsion), for intravenous use and Intralipid® 30% (A 30% I.V. Fat Emulsion) can be found at www.FreseniusKabiNutrition.com/Intralipid20PI and www.FreseniusKabiNutrition.com/Intralipid30PI.
For Healthcare Professionals
Intralipid (lipid injectable emulsion) for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
Intralipid 20% (A 20% Intravenous Fat Emulsion), is indicated as a source of calories and essential fatty acids for patients requiring parenteral nutrition (PN) and as a source of essential fatty acids for prevention of essential fatty acid deficiency (EFAD).
Intralipid 20% Pharmacy Bulk Package and Intralipid 30% Pharmacy Bulk Package are intended for use in a pharmacy admixture program for the preparation of three-in-one or total nutrition admixtures (TNAs) to provide a source of calories and essential fatty acids for adult and pediatric patients requiring PN and a source of essential fatty acids for prevention of EFAD.
INTRALIPID 20% and 30% PHARMACY BULK PACKAGES ARE NOT INTENDED FOR DIRECT INTRAVENOUS ADMINISTRATION.
IMPORTANT SAFETY INFORMATION
INTRALIPID 20% (A 20% INTRAVENOUS FAT EMULSION) PHARMACY BULK PACKAGE AND INTRALIPID 30% (A 30% INTRAVENOUS FAT EMULSION) PHARMACY BULK PACKAGE IS NOT INTENDED FOR DIRECT INTRAVENOUS ADMINISTRATION. DILUTING INTRALIPID 20% TO A 10% CONCENTRATION OR 30% TO A 10% OR 20% CONCENTRATION WITH AN INTRAVENOUS FLUID SUCH AS NORMAL SALINE OR OTHER DILUENT DOES NOT PRODUCE A DILUTION THAT IS EQUIVALENT IN COMPOSITION TO INTRALIPID 10% OR 20% I.V. FAT EMULSIONS, AND SUCH A DILUTION SHOULD NOT BE GIVEN BY DIRECT INTRAVENOUS ADMINISTRATION.
Recommended dosage depends on age, energy expenditure, clinical status, body weight, tolerance, ability to metabolize and eliminate lipids, and consideration of additional energy given to the patient. Protect the admixed PN solution from light. Use a 1.2 micron in-line filter during administration.
Dosage for Intralipid 20%
| Age | Nutritional Requirements | |
|---|---|---|
| Initial Recommended Dosage | Maximum Dosage | |
| Birth to 2 years of age (including preterm and term neonates) |
0.5 g/kg/day | 3 g/kg/day |
| Pediatric patients 2 to <12 years of age | 1 to 2 g/kg/day | 2.5 g/kg/day |
| Pediatric patients 12 to 17 years of age | 1 g/kg/day | 2 g/kg/day |
| Adults | 1 g/kg/day (stable) ≤1 g/kg/day (critically ill) |
2.5 g/kg/day |
Dosage for Intralipid 30%
Premature infants: initial dose at 0.5 g/kg/24 hours, maximum recommended dosage is 3g fat/kg/24 hours.
Older pediatric patients: daily dose should not exceed 3 of g fat/kg/d.
Adults: The daily dosage should not exceed 2.5 g of fat/kg of body weight
Intralipid is contraindicated in patients with:
- Known hypersensitivity to egg, soybean, or peanut, or any of the active ingredients or excipients.
- Severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglyceride > 1,000 mg/dL).
- Disturbances of normal fat metabolism such as pathologic hyperlipemia, lipoid nephrosis or acute pancreatitis if accompanied by hyperlipidemia.
Risk of Clinical Decompensation with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Risk of Parenteral Nutrition-Associated Liver Disease (PNALD): Increased risk in patients who receive PN for extended periods of time, especially preterm neonates. Monitor liver function tests; if abnormalities occur consider discontinuation or dosage reduction.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reactions occur.
Risk of Infections, Fat Overload Syndrome, Refeeding Syndrome, and Hypertriglyceridemia: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm neonates.
Most common adverse drug reactions (≥5%) from clinical trials in adults were nausea, vomiting, and pyrexia. Most common adverse drug reactions (≥5%) from clinical trials in pediatric patients were anemia, vomiting, increased gamma-glutamyltransferase, and cholestasis.
Vitamin K Antagonists (e.g., warfarin): Anticoagulant activity may be counteracted; increase monitoring of coagulation parameters.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use Intralipid safely and effectively. Please see full prescribing information for Intralipid 20% (lipid injectable emulsion), for intravenous use and Intralipid® 30% (A 30% I.V. Fat Emulsion) can be found at www.FreseniusKabiNutrition.com/Intralipid20PI and www.FreseniusKabiNutrition.com/Intralipid30PI.
For Consumers
SMOFLIPID® (lipid injectable emulsion USP), for intravenous use
IMPORTANT SAFETY INFORMATION
What is SMOFlipid?
- Indicated in adult and pediatric patients as a source of calories and essential fatty acids for parenteral nutrition (PN) when oral or enteral nutrition is not possible, insufficient, or contraindicated.
- The hourly infusion rate in pediatrics should not exceed 0.75 mL/kg/hour and 0.5 mL/kg/hour in adults.
SMOFlipid should not be received by patients who have:
- A known allergy to fish, egg, soybean, or peanut, or to any of the active or inactive ingredients in SMOFlipid.
- Abnormally high levels of lipid (triglycerides) in the blood.
SMOFlipid may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Parenteral nutrition-associated liver disease (PNALD) may progress to liver inflammation and damage caused by a buildup of fat in the liver with scarring and cirrhosis.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides (Hypertriglyceridemia): Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels.
Monitoring/Laboratory Tests: The content of vitamin K may interfere with blood clotting activity of medications.
The most common side effects (>1%) in adult patients include nausea, vomiting, and high levels of glucose in the blood and in pediatric patients include low levels of red blood cells, vomiting, increased levels of liver enzymes (i.e., gamma-glutamyltransferase) and hospital-acquired infections.
These are not all the possible side effects associated with SMOFlipid. Call your healthcare provider for medical advice regarding SMOFlipid side effects. You are encouraged to report negative side effects of SMOFlipid. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling can be found at https://www.FreseniusKabiNutrition/SMOFlipidPI.
For Healthcare Professionals
SMOFLIPID (lipid injectable emulsion, USP), for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
SMOFlipid is indicated in adult and pediatric patients, including term and preterm neonates, as a source of calories and essential fatty acids for parenteral nutrition (PN) when oral or enteral nutrition is not possible, insufficient, or contraindicated.
IMPORTANT SAFETY INFORMATION
For intravenous infusion only into a central or peripheral vein. Use a non-vented non-DEHP 1.2 micron in-line filter set during administration. Recommended dosage depends on age, energy expenditure, clinical status, body weight, tolerance, ability to metabolize and eliminate lipids, and consideration of additional energy given to the patient. The recommended dose for adults and pediatrics is shown in Table 1. For information on age-appropriate infusion rate, see the full prescribing information. SMOFlipid Pharmacy Bulk Package is only indicated for use in pharmacy admixture programs for the preparation of three-in-one or total nutrition admixtures. Protect the admixed PN solution from light.
Table 1: Recommended Adult and Pediatric Dosage
| Age | Nutritional Requirements | |
|---|---|---|
| Initial Recommended Dosage | Maximum Dosage | |
| Birth to 2 years of age (including preterm and term neonates) |
0.5 to 1 g/kg/day | 3 g/kg/day |
| Pediatric patients 2 to <12 years of age | 1 to 2 g/kg/day | 3 g/kg/day |
| Pediatric patients 12 to 17 years of age | 1 g/kg/day | 2.5 g/kg/day |
| Adults | 1 to 2 g/kg/day | 2.5 g/kg/day |
SMOFlipid is contraindicated in patients with known hypersensitivity to fish, egg, soybean, peanut, or any of the active or inactive ingredients, and severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglycerides >1,000 mg/dL).
Clinical Decompensation with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who received parenteral nutrition for greater than 2 weeks, especially preterm neonates. Monitor liver tests; if abnormalities occur consider discontinuation or dosage reduction.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reactions occur.
Risk of Infections, Fat Overload Syndrome, Refeeding Syndrome, Hypertriglyceridemia, and Essential Fatty Acid Deficiency: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm neonates.
Most common adverse drug reactions (≥5%) from clinical trials in adults were nausea, vomiting, and hyperglycemia. Most common adverse drug reactions (≥5%) from clinical trials in pediatric patients were anemia, vomiting, increased gamma-glutamyltransferase, and nosocomial infection.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use SMOFlipid safely and effectively. Please see full prescribing information for SMOFlipid (lipid injectable emulsion, USP), for intravenous use at www.FreseniusKabiNutrition.com/SMOFlipidPI.
For Consumers
OMEGAVEN (fish oil triglycerides) injectable emulsion, for intravenous use
IMPORTANT SAFETY INFORMATION
These highlights do not include all the information needed to use OMEGAVEN safely and effectively. To learn more about OMEGAVEN for your child, talk to your child’s healthcare provider. OMEGAVEN is available by prescription only. The FDA-approved product labeling can be found at www.freseniuskabinutrition.com/OmegavenPI.
What is OMEGAVEN?
- A fish oil-based intravenous lipid emulsion that is a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis (PNAC).
- Does not prevent PNAC.
- It has not been demonstrated that the clinical outcomes seen in pediatric patients are a result of the omega-6:omega-3 fatty acid ratio of the product.
- The hourly infusion rate should not exceed 1.5 mL/kg/hour
OMEGAVEN should not be received by patients who have:
- a known allergy to fish or egg protein or to any of the ingredients in OMEGAVEN.
- a severe bleeding disorder.
- abnormally high levels of lipid (triglycerides) in the blood.
What important safety information should I know about OMEGAVEN?
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides (Hypertriglyceridemia): Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels.
The most common side effects, (>15%) include: vomiting, agitation, slower than normal heartbeat, interruption of breathing, and viral infection.
These are not all the possible side effects associated with OMEGAVEN. Call your healthcare provider for medical advice regarding OMEGAVEN side effects. You are encouraged to report negative side effects of OMEGAVEN. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling can be found at www.FreseniusKabiNutrition.com/OmegavenPI.
For Healthcare Professionals
OMEGAVEN (fish oil triglycerides) injectable emulsion, for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
Omegaven is indicated as a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis (PNAC).
Limitations of Use
Omegaven is not indicated for the prevention of PNAC. It has not been demonstrated that Omegaven prevents PNAC in parenteral nutrition (PN)-dependent patients.
It has not been demonstrated that the clinical outcomes observed in patients treated with Omegaven are a result of the omega-6: omega-3 fatty acid ratio of the product.
IMPORTANT SAFETY INFORMATION
Protect the admixed PN solution from light. Prior to administration, correct severe fluid and electrolyte disorders and measure serum triglycerides to establish a baseline level. Initiate dosing in PN-dependent pediatric patients as soon as direct or conjugated bilirubin levels are 2 mg/dL or greater. The recommended nutritional requirements of fat and recommended dosages of Omegaven to meet those requirements for pediatric patients are provided in Table 1, along with recommendations for the initial and maximum infusion rates. Administer Omegaven until direct or conjugated bilirubin levels are less than 2 mg/dL or until the patient no longer requires PN.
Table 1: Recommended Pediatric Dosage and Infusion Rate
| Nutritional Requirements | Direct Infusion Rate | |
|---|---|---|
| Initial | Maximum | |
| 1 g/kg/day; this is also the maximum daily dose | 0.2 mL/kg/hour for the first 15 to 30 minutes; gradually increase to the required rate after 30 minutes |
1.5 mL/kg/hour |
Omegaven is contraindicated in patients with known hypersensitivity to fish or egg protein or to any of the active ingredients or excipients, severe hemorrhagic disorders due to a potential effect on platelet aggregation, severe hyperlipidemia or severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglyceride concentrations greater than 1,000 mg/dL).
Clinical Decompensation with Rapid Infusion of Lipid Injectable Emulsions in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported. Hypertriglyceridemia was commonly reported. Strictly adhere to the recommended total daily dosage; the hourly infusion rate should not exceed 1.5 mL/kg/hour. Carefully monitor the infant’s ability to eliminate the infused lipids from the circulation (e.g., measure serum triglycerides and/or plasma free fatty acid levels). If signs of poor clearance of lipids from the circulation occur, stop the infusion and initiate a medical evaluation.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reaction occurs.
Infections, Fat Overload Syndrome, Refeeding Syndrome, and Hypertriglyceridemia: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm infants.
Monitoring and Laboratory Tests: Routine laboratory monitoring is recommended, including monitoring for essential fatty acid deficiency.
The most common adverse drug reactions (>15%) are: vomiting, agitation, bradycardia, apnea and viral infection.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use Omegaven safely and effectively. Please see full prescribing information for Omegaven (fish oil triglycerides) injectable emulsion for intravenous use at www.freseniuskabinutrition.com/OmegavenPI.
For Consumers
KABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
PERIKABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
IMPORTANT SAFETY INFORMATION
What is Kabiven and Perikabiven?
- Indicated in adult patients as a source of calories, protein, electrolytes and essential fatty acids for parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. Kabiven and Perikabiven may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adults.
- Do not exceed the recommended maximum infusion rate of 2.6 mL/kg/hour for Kabiven and 3.7 mL/kg/hour for Perikabiven.
Limitations of Use
Neither Kabiven nor Perikabiven is recommended in pediatric patients less than 2 years old because the fixed amount of the formulations do not meet nutritional needs in this age group.
Do not use Kabiven or Perikabiven in patients who have:
- Simultaneous treatment with ceftriaxone in neonates (28 days of age or younger)
- Known allergy to egg, soybean, peanut or any of the active or inactive ingredients
- Abnormally high levels of lipid (triglycerides) in the blood (with serum triglyceride concentration >1,000 g/dL)
- Inborn errors of amino acid metabolism (a genetic defect in protein metabolism)
- Cardiopulmonary instability (inability for the heart and lungs to function right)
- Hemophagocytic syndrome (a disorder of the immune system)
Kabiven and Perikabiven may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly follow the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who receive parenteral nutrition for greater than 2 weeks. Your healthcare provider will monitor liver tests.
- Pulmonary Embolism (a blockage in a blood vessel in the lung) and Respiratory Distress (increased breathing rate, bluish skin color changes, wheezing) due to Pulmonary Vascular Precipitates (solid substance in the blood vessel of the lungs): If signs of lung issues occur, stop the infusion and start a medical evaluation.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction
- Precipitation (solid substance in the blood vessel) with Ceftriaxone: Do not administer ceftriaxone simultaneously with Kabiven or Perikabiven via a Y-site.
- Infection, fat overload, hyperglycemia (high blood sugar) and refeeding syndrome: Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels
The most common adverse reactions for Kabiven (≥3%) are nausea, fever, high blood pressure, vomiting, decreased blood hemoglobin, decreased blood total protein, low blood potassium, and increased gamma glutamyltransferase (a liver enzyme). The most common adverse reactions for Perikabiven (≥3%) are high blood sugar, low blood potassium, fever and increased blood lipids.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Tell your doctor if you are taking coumarin and coumarin derivatives, including warfarin: the drug activity may be lessened and your healthcare provider will monitor your blood.
These are not all the possible side effects associated with Kabiven and Perikabiven. Call your healthcare provider for medical advice regarding Kabiven and Perikabiven side effects. You are encouraged to report negative side effects of Kabiven and Perikabiven. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling for KABIVEN® (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use and PERIKABIVEN® (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use can be found at www.FreseniusKabiNutrition.com/KabivenPI and www.FreseniusKabiNutrition.com/PerikabivenPI.
For Healthcare Professionals
KABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
PERIKABIVEN (Amino Acids, Electrolytes, Dextrose, and Lipid Injectable Emulsion), for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
KABIVEN and PERIKABIVEN are each indicated as a source of calories, protein, electrolytes and essential fatty acids for adult patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. KABIVEN and PERIKABIVEN may be used to prevent essential fatty acid deficiency or treat negative nitrogen balance in adult patients.
Limitations of Use
Neither KABIVEN nor PERIKABIVEN is recommended for use in pediatric patients <2 years including preterm infants because the fixed content of the formulation does not meet nutritional requirements in this age group.
IMPORTANT SAFETY INFORMATION
KABIVEN is indicated for intravenous infusion into a central vein. PERIKABIVEN is indicated for intravenous infusion into a peripheral or central vein. It is recommended to mix the contents thoroughly by inverting the bags upside down to ensure a homogenous admixture. Ensure the vertical seals between chambers are broken and the contents of all three chambers for KABIVEN and PERIKABIVEN are mixed together prior to infusion. The dosage of KABIVEN and PERIKABIVEN should be individualized based on the patient’s clinical condition (ability to adequately metabolize amino acids, dextrose and lipids), body weight and nutritional/fluid requirements, as well as additional energy given orally/enterally to the patient. Prior to administration of KABIVEN and PERIKABIVEN, correct severe fluid, electrolyte and acid-base disorders. Before starting the infusion, obtain serum triglyceride levels to establish the baseline value. Do not exceed the recommended maximum infusion rate of 2.6 mL/kg/hour for KABIVEN and 3.7 mL/kg/hour for PERIKABIVEN.
KABIVEN and PERIKABIVEN are contraindicated in:
- Concomitant treatment with ceftriaxone in neonates (28 days of age or younger)
- Known hypersensitivity to egg, soybean, peanut, or any of the active or inactive ingredients.
- Severe disorders of lipid metabolism characterized by hypertriglyceridemia (with serum triglyceride concentration >1,000 g/dL).
- Inborn errors of amino acid metabolism.
- Cardiopulmonary instability
- Hemophagocytic syndrome
Clinical Decompensation with Rapid Infusion of Lipid Injectable Emulsions in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Parenteral Nutrition-Associated Liver Disease: Increased risk in patients who receive parenteral nutrition for greater than 2 weeks. Monitor liver tests; if abnormalities occur, consider discontinuation or dosage reduction.
Pulmonary Embolism and Respiratory Distress due to Pulmonary Vascular Precipitates: If signs of pulmonary distress occur, stop the infusion and initiate a medical evaluation.
Hypersensitivity reactions: Monitor for signs or symptoms and discontinue infusion if reactions occur.
Precipitation with Ceftriaxone: Do not administer ceftriaxone simultaneously with KABIVEN or PERIKABIVEN via a Y-site.
Infection, fat overload, hyperglycemia and refeeding complications: Monitor for signs and symptoms; monitor laboratory parameters.
The most common adverse reactions for KABIVEN (≥3%) are nausea, pyrexia, hypertension, vomiting, decreased hemoglobin, decreased total protein, hypokalemia, decreased potassium, and increased gamma glutamyltransferase. The most common adverse reactions for PERIKABIVEN (≥3%) are hyperglycemia, hypokalemia, pyrexia, and increased blood triglycerides.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Coumarin and coumarin derivatives, including warfarin: Anticoagulant activity may be counteracted; monitor laboratory parameters
This Important Safety Information does not include all the information needed to use KABIVEN and PERIKABIVEN safely and effectively. Please see full prescribing information for KABIVEN and PERIKABIVEN (amino acids, electrolytes, dextrose and lipid injectable emulsion), for intravenous use at www.FreseniusKabiNutrition.com/KabivenPI and www.FreseniusKabiNutrition.com/PerikabivenPI.
For Consumers
Intralipid (lipid injectable emulsion) for intravenous use
IMPORTANT SAFETY INFORMATION
What is Intralipid?
- Indicated as a source of calories and essential fatty acids for adult and pediatric patients requiring parenteral nutrition (PN) and as a source of essential fatty acids for prevention of essential fatty acid deficiency (EFAD).
Intralipid should not be received by patients who have:
- A known allergy to egg, soybean, or peanut, or any of the active ingredients or excipients in Intralipid.
- Abnormally high levels of lipid (triglycerides) in the blood.
Intralipid may cause serious side effects including:
- Serious Adverse Reactions with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Strictly adhere to the recommended total daily dosage and do not exceed the maximum infusion rate. If poor clearance of fats occurs, the infusion should be stopped, and a medical evaluation started.
- Risk of Parenteral Nutrition-Associated Liver Disease: Parenteral nutrition-associated liver disease (PNALD) may progress to liver inflammation and damage caused by a buildup of fat in the liver with scarring and cirrhosis.
- Allergic Reactions: Contact your healthcare provider immediately if you are experiencing an allergic reaction.
- Fat Overload Syndrome, Refeeding Syndrome, Elevated Triglycerides: Your healthcare provider will monitor you for signs and symptoms of early infection and blood levels
Monitoring/Laboratory Tests: The content of vitamin K may interfere with blood clotting activity of medications.
The most common side effects (≥5%) in adult patients include nausea, vomiting and fever and in pediatric patients include low levels of red blood cells, vomiting, increased levels of liver enzymes (i.e., gamma-glutamyltransferase), and cholestasis (i.e., reducing or blocking the flow of bile).
These are not all the possible side effects associated with Intralipid. Call your healthcare provider for medical advice regarding Intralipid side effects. You are encouraged to report negative side effects of Intralipid. Contact Fresenius Kabi USA, LLC at: 1-800-551-7176 or FDA at: 1-800-FDA-1088 or www.fda.gov/medwatch. The FDA-approved product labeling for Intralipid® 20% (lipid injectable emulsion), for intravenous use and Intralipid® 30% (A 30% I.V. Fat Emulsion) can be found at www.FreseniusKabiNutrition.com/Intralipid20PI and www.FreseniusKabiNutrition.com/Intralipid30PI.
For Healthcare Professionals
Intralipid (lipid injectable emulsion) for intravenous use
IMPORTANT SAFETY INFORMATION
INDICATIONS AND USAGE
Intralipid 20% (A 20% Intravenous Fat Emulsion), is indicated as a source of calories and essential fatty acids for patients requiring parenteral nutrition (PN) and as a source of essential fatty acids for prevention of essential fatty acid deficiency (EFAD).
Intralipid 20% Pharmacy Bulk Package and Intralipid 30% Pharmacy Bulk Package are intended for use in a pharmacy admixture program for the preparation of three-in-one or total nutrition admixtures (TNAs) to provide a source of calories and essential fatty acids for adult and pediatric patients requiring PN and a source of essential fatty acids for prevention of EFAD.
INTRALIPID 20% and 30% PHARMACY BULK PACKAGES ARE NOT INTENDED FOR DIRECT INTRAVENOUS ADMINISTRATION.
IMPORTANT SAFETY INFORMATION
INTRALIPID 20% (A 20% INTRAVENOUS FAT EMULSION) PHARMACY BULK PACKAGE AND INTRALIPID 30% (A 30% INTRAVENOUS FAT EMULSION) PHARMACY BULK PACKAGE IS NOT INTENDED FOR DIRECT INTRAVENOUS ADMINISTRATION. DILUTING INTRALIPID 20% TO A 10% CONCENTRATION OR 30% TO A 10% OR 20% CONCENTRATION WITH AN INTRAVENOUS FLUID SUCH AS NORMAL SALINE OR OTHER DILUENT DOES NOT PRODUCE A DILUTION THAT IS EQUIVALENT IN COMPOSITION TO INTRALIPID 10% OR 20% I.V. FAT EMULSIONS, AND SUCH A DILUTION SHOULD NOT BE GIVEN BY DIRECT INTRAVENOUS ADMINISTRATION.
Recommended dosage depends on age, energy expenditure, clinical status, body weight, tolerance, ability to metabolize and eliminate lipids, and consideration of additional energy given to the patient. Protect the admixed PN solution from light. Use a 1.2 micron in-line filter during administration.
Dosage for Intralipid 20%
| Age | Nutritional Requirements | |
|---|---|---|
| Initial Recommended Dosage | Maximum Dosage | |
| Birth to 2 years of age (including preterm and term neonates) |
0.5 g/kg/day | 3 g/kg/day |
| Pediatric patients 2 to <12 years of age | 1 to 2 g/kg/day | 2.5 g/kg/day |
| Pediatric patients 12 to 17 years of age | 1 g/kg/day | 2 g/kg/day |
| Adults | 1 g/kg/day (stable) ≤1 g/kg/day (critically ill) |
2.5 g/kg/day |
Dosage for Intralipid 30%
Premature infants: initial dose at 0.5 g/kg/24 hours, maximum recommended dosage is 3g fat/kg/24 hours.
Older pediatric patients: daily dose should not exceed 3 of g fat/kg/d.
Adults: The daily dosage should not exceed 2.5 g of fat/kg of body weight
Intralipid is contraindicated in patients with:
- Known hypersensitivity to egg, soybean, or peanut, or any of the active ingredients or excipients.
- Severe disorders of lipid metabolism characterized by hypertriglyceridemia (serum triglyceride > 1,000 mg/dL).
- Disturbances of normal fat metabolism such as pathologic hyperlipemia, lipoid nephrosis or acute pancreatitis if accompanied by hyperlipidemia.
Risk of Clinical Decompensation with Rapid Infusion of Intravenous Lipid Emulsion in Neonates and Infants: Acute respiratory distress, metabolic acidosis, and death after rapid infusion of intravenous lipid emulsions have been reported.
Risk of Parenteral Nutrition-Associated Liver Disease (PNALD): Increased risk in patients who receive PN for extended periods of time, especially preterm neonates. Monitor liver function tests; if abnormalities occur consider discontinuation or dosage reduction.
Hypersensitivity Reactions: Monitor for signs or symptoms. Discontinue infusion if reactions occur.
Risk of Infections, Fat Overload Syndrome, Refeeding Syndrome, and Hypertriglyceridemia: Monitor for signs and symptoms; monitor laboratory parameters.
Aluminum Toxicity: Increased risk in patients with renal impairment, including preterm neonates.
Most common adverse drug reactions (≥5%) from clinical trials in adults were nausea, vomiting, and pyrexia. Most common adverse drug reactions (≥5%) from clinical trials in pediatric patients were anemia, vomiting, increased gamma-glutamyltransferase, and cholestasis.
Vitamin K Antagonists (e.g., warfarin): Anticoagulant activity may be counteracted; increase monitoring of coagulation parameters.
To report SUSPECTED ADVERSE REACTIONS, contact Fresenius Kabi USA, LLC at 1-800-551-7176, option 5, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
This Important Safety Information does not include all the information needed to use Intralipid safely and effectively. Please see full prescribing information for Intralipid 20% (lipid injectable emulsion), for intravenous use and Intralipid® 30% (A 30% I.V. Fat Emulsion) can be found at www.FreseniusKabiNutrition.com/Intralipid20PI and www.FreseniusKabiNutrition.com/Intralipid30PI.